What is Thyroid cancer?
One kind of cancer that arises in the cells of the thyroid gland—which is situated in the front of the neck, directly on the Windpipe—is called thyroid cancer. Hormones produced by the thyroid gland regulate heart rate, metabolism, and other vital body functions.
Thyroid cancer comes in four primary forms, the majority of which originate from the follicular cells that produce thyroid hormone.
Papillary Thyroid Carcinoma: Making up over 80% of cases, papillary carcinoma is the most prevalent form of thyroid cancer. It is a slow growing cancer. It can spread to neighbouring lymph nodes and rarely to the sound box nerve and voice box. This group generally have excellent cure rates if treated properly.
Follicular Thyroid Carcinoma: Accounting for 10–15% of cases, follicular carcinoma is the second most prevalent form of thyroid cancer. It starts in the thyroid gland’s follicular cells and has the potential involve blood vessels and have a propensity to spread to lungs, bones, spine… The prognosis for follicular thyroid carcinoma is generally favourable, even when there is spread to distant sites. The key to achieve good results is a good surgery and appropriate adjuvant treatment.
Medullary Thyroid Carcinoma: The thyroid gland’s parafollicular cells (C cells), which generate the hormone calcitonin, are the source of medullary carcinoma. Roughly 4-5% of thyroid malignancies are caused by it. Compared to papillary and follicular thyroid cancers, medullary thyroid cancer typically spreads to lymph nodes. It may manifest intermittently or in conjunction with multiple endocrine neoplasia (MEN), a hereditary condition. Surgery for an important first treatment in these cancers, additional treatment in form of radiotherapy may me needed in advanced cases.
Anaplastic Thyroid Carcinoma: Anaplastic carcinoma accounts for 1%–2% of thyroid cancer cases and is an uncommon but severe form of the disease. It spreads quickly and frequently shows resistance to therapy. The prognosis for anaplastic thyroid carcinoma is often poor, with a low survival rate.
In addition, around 5% of thyroid cancer cases are Poorly Differentiated Thyroid Cancer, which typically affects older adults. Often, it may not be iodine-avid.
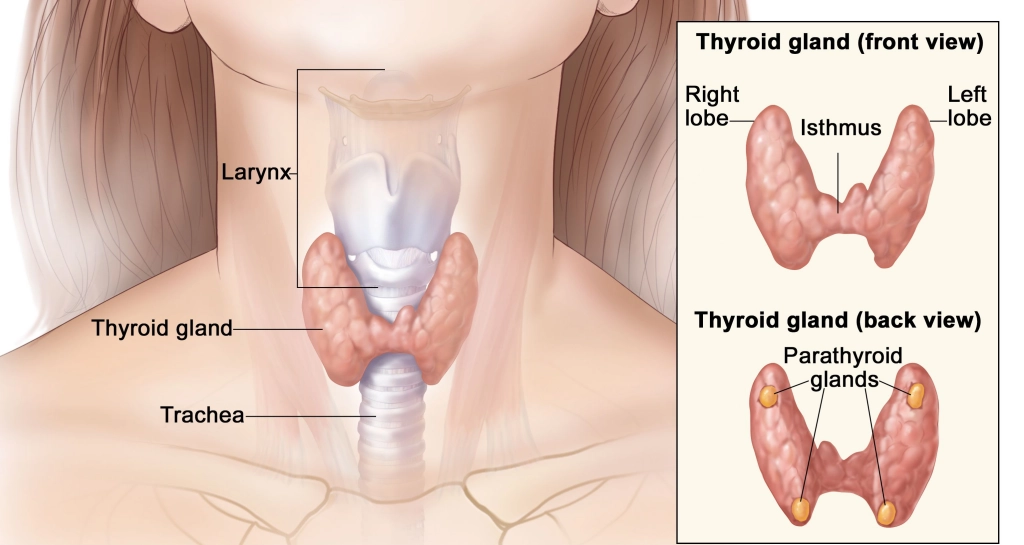
Thyroid gland
Everyone has a thyroid gland and it is present in the lower part of neck in midline. It has a butterfly-like shape and encircles the trachea, which is the windpipe, below the larynx (sound box).
Parts of thyroid are
- Wings of the butterfly (left and right lobes)
- Body of the buuterfly(isthmus, connecting the left and right lobes)
- Small part lying over the voice box (pyramidal lobe).
A goitre is the term used to describe an enlarged thyroid. Nodules are the term for lumps in the thyroid. While most thyroid nodules are benign, some may develop into malignancy.
Functions of thyroid
Endocrine glands are those that release hormones into the bloodstream; the thyroid is the body’s largest endocrine gland.
- Hormones produced by the thyroid are transported to all bodily tissues by the blood.
- Thyroxine (T4) and tri-iodothyronine (T3) are the two forms of thyroid hormone.
- These hormones are crucial for brain function because they regulate metabolism, the rate at which cells function.
- These hormones are crucial for children’s brain development and growth because they regulate metabolism, the rate at which cells function.
- The sensitivity of other organs to endocrine hormones is also regulated by these hormones.
- Follicular cells are the cells that produce thyroid hormone.
- The pituitary gland regulates the blood’s concentration of thyroid hormone. Located beneath the brain is a small endocrine gland called the pituitary.
- Thyroid stimulating hormone (TSH) is released into the bloodstream by it. All three of these hormones (TSH, T4, and T3) are examined when doctors order thyroid tests, but TSH is the most crucial.
- Overactive thyroid, often known as hyperthyroidism, is the result of excessive thyroid hormone.Heart palpitations, difficulty falling asleep, trembling hands, weakened muscles, uneasiness or worry, feeling warm, and issues with your menstrual cycle can result from this.
- Hypothyroidism, often known as an underactive thyroid, is the absence of adequate thyroid hormone. Weight gain, sluggishness, a cold intolerance, depression, constipation, issues with hair loss, and a dry thyroid can result from this.
Causes of thyroid cancer
Thyroid cancer’s precise cause is frequently unknown. Nonetheless, a number of variables could raise the chance of thyroid cancer, such as:
- Radiation exposure, particularly as a youngster.
- Thyroid cancer in the family history or specific genetic disorders like familial adenomatous polyposis or familial medullary thyroid cancer.
- Gender (thyroid cancer is more common in women than in males).
- Age (those over 40 are more likely to develop thyroid cancer).
Symptoms of thyroid cancer
Early-stage thyroid cancer may not exhibit any symptoms. The following symptoms could appear when the cancer spreads:
- A lump or swelling in the neck (a thyroid nodule).
- Voice changes or hoarseness.
- Breathing or swallowing difficulties.
- Persistent cough that is not related to the common cold.
- Either lymph node swelling or pain in the neck.
Tests for thyroid cancer
- Physical Exam: A medical Physical Examination: To look for any lumps or swelling in the neck, a medical professional may conduct a physical examination.
- Imaging Tests: The thyroid gland can be seen, and any nodules or masses can be identified by size and characteristics using imaging tests like Ultrasound of Neck. CT Neck with contrast is done in patients presenting with lymph nodes, voice change or involvement of the sound box.
- USG guided FNAC: In a FNAC, few cells from the thyroid lump or nodule is taken under Ultrasound guidance, and it is examined under a microscope to look for pathology.
Treatment for thyroid cancer
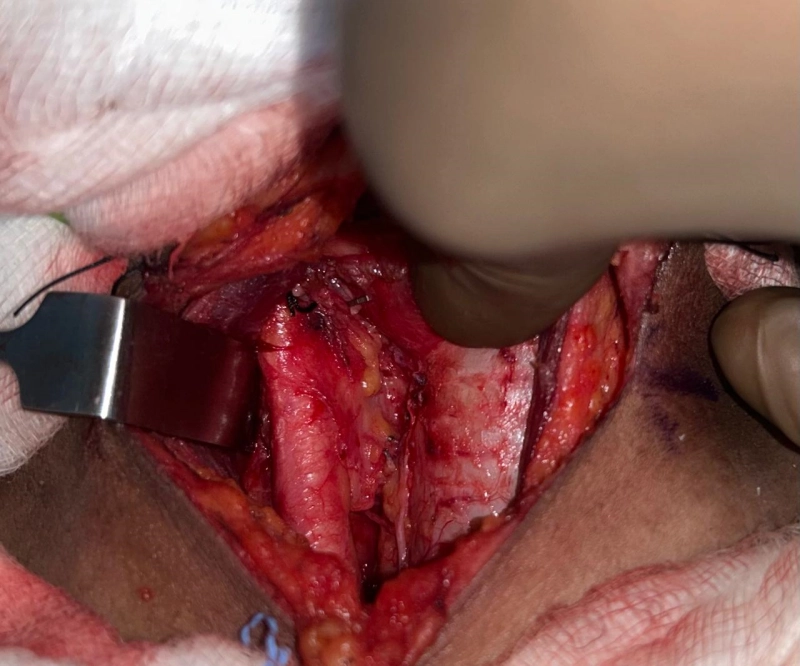
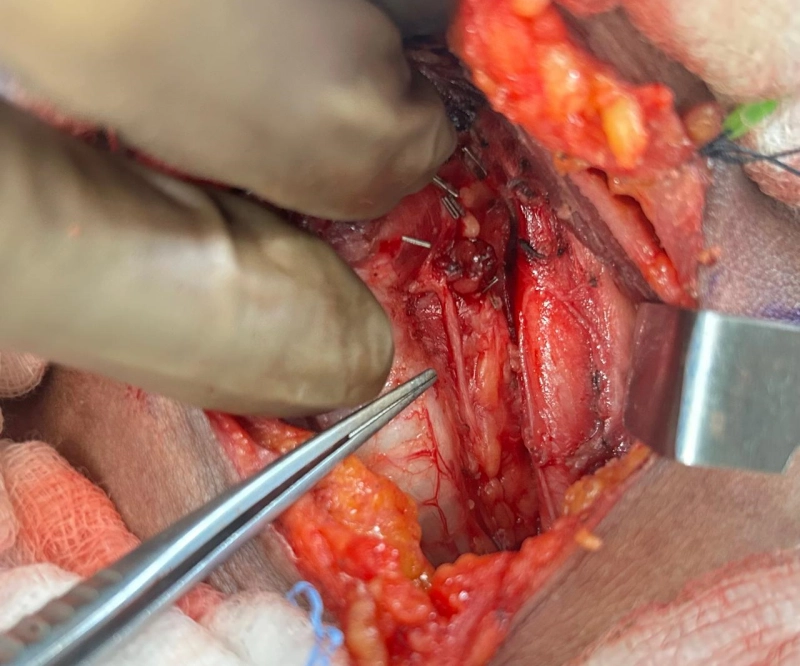
Surgery (Hemithyroidectomy / Total thyroidectomy) forms the first and the most important preferred treatment modality in thyroid cancers. This will be followed by the additional adjuvant treatment options discussed below.
- Surgery: Thyroidectomy, which entails the surgical removal of all or part of the thyroid, is the most popular treatment for thyroid cancer. Thyroidectomy, in which the thyroid gland is surgically removed entirely or in part. If cancerous cells are found in the neck lymph nodes, these may also need to be removed. In surgery of thyroid, functional preservation of the sound box nerve and parathyroid preservation is important along with complete removal of thyroid gland and lymph nodes if involved.
- After surgery, radioactive iodine therapy can be utilised to eradicate any cancer cells or thyroid tissue that may still be present. Thyroid cancer, both follicular and papillary, is frequently treated with this medication.
- Thyroid Hormone Replacement Therapy: To restore the hormones that the thyroid gland normally produces, thyroid hormone replacement therapy is typically required following a thyroidectomy.
- Radioactive iodine therapy: Is the adjuvant therapy advised after Total thyroidectomy to destroy the microscopic thyroid cells. The medications is consumed in the form of capsule or drink and the remnant microscopic thyroid cells pick up the iodine and gets destroyed. Even if the thyroid cancer has spread to other parts of the body, it will get deposited and control or cure the cancer.
- External Beam Radiation Therapy: Radiation therapy can be used as adjuvant therapy in some advanced cancers or palliative care for advanced thyroid cancer or to treat thyroid cancer that has spread to surrounding tissues.